REVIEW ARTICLE | https://doi.org/10.5005/jp-journals-10084-12143 |
A Global Threat COVID-19: Understanding and its Management
1Department of Medical and Surgical Nursing, Narayana Hrudayalaya College of Nursing, Bengaluru, Karnataka, India
2Department of Nursing, Government Mohan Kumaramangalam Medical College and Hospital, Salem, Tamil Nadu, India
3Department of Nursing, Aliaa Specialist Hospital, Omdurman, Khartoum, Sudan
Corresponding Author: Puvaneswari Kanagaraj, Department of Medical and Surgical Nursing, Narayana Hrudayalaya College of Nursing, Bengaluru, Karnataka, India, Phone: +91 9448126938, e-mail: puvaneswariramesh@gmail.com
How to cite this article Kanagaraj P, Kanagaraj A, Yesuwilson AJ. A Global Threat COVID-19: Understanding and its Management. Pon J Nurs 2020;13(1):18–21.
Source of support: Nil
Conflict of interest: None
ABSTRACT
COVID-19 disease is a highly infectious disease caused by a newly (novel) identified corona virus. COVID-19 infected patients may have mild to moderate respiratory symptoms and can recover without any specific medical management. But few experience severe symptoms and lead to mortality. COVID-19 is announced by WHO as a global pandemic. It is very critical to take appropriate decisions and timely management and prevention of the infection.
Keywords: COVID-19, Diagnostic test, Management of COVID19, Pandemic, Pathophysiology, Signs, Symptoms.
INTRODUCTION
Corona viruses can affect birds, mammals, and also human beings (identified in 1960).1 The term “Corona virus” is obtained from a word “Corona” from Latin meaning “crown” or “wreath.”2 Some of the corona infections identified were SARS-CoV (2003), HCoV NL63 (2004), and MERS-CoV (2012).3 On February 11, 2020, the WHO has announced unexplained low respiratory infections detected in Wuhan city, China, i.e., named as “Coronavirus disease 2019,” an acronym of COVID-19, which is caused by a novel CoV.4
DEFINITION
COVID-19 is a pandemic disease caused by COVID-19 or SARS-CoV-2, which is genetically similar to the severe acute respiratory syndrome (SARS) coronavirus.5
TRANSMISSION, INCUBATION PERIOD, AND VULNERABLE GROUPS
COVID-19 primarily spreads through the respiratory tract by droplets (cough and sneeze), respiratory secretions, and direct contact.6 People become infected with COVID-19 by touching the contaminated objects or surfaces with COVID 19, then touching their eyes, nose, or mouth.7 COVID-19 infection has an incubation period of 1–14 days, mostly 3–7 days.8 It is highly transmissible in humans. People who are older or who have existing chronic medical conditions, such as hypertension, compromised lung function, chronic obstructive pulmonary disease or diabetes, cancer, or who have compromised immune systems may be at higher risk of serious illness.9–11
PATHOPHYSIOLOGY4,12–14
A pathophysiology and virulence mechanism of COVID-19 has a link to the function of structural and nonstructural proteins. The pathophysiology is explained in Flowchart 1.
CLINICAL MANIFESTATIONS/SYNDROMES IN ADULTS15,16
The clinical features of coronavirus disease-19 can vary from asymptomatic to severe clinical conditions. Clinical syndromes are explained in Figure 1.
DIAGNOSTIC TESTS17,18
Use appropriate personal protective equipment (PPE) while taking specimens like blood, upper, and lower respiratory samples. Follow droplet, contact, and airborne precautions. It is explained in Figure 2.
MANAGEMENT15,16
Clinical Management15,16
Infection Prevention and Control Measures
- Infection prevention and control (IPC) measures need to be initiated along with the screening and give a mask to the suspected COVID-19 and direct to separate area with 1-m distance between patient to patient.
- Healthcare workers should follow the standard precautions (hand hygiene, appropriate PPE, biomedical waste management, prevention of needle-stick injury, cleaning and disinfection of equipment and environment when in contact with body fluids, blood, secretions (respiratory), and nonintact skin both directly or indirectly.

Flowchart 1: Pathophysiology of COVID-19
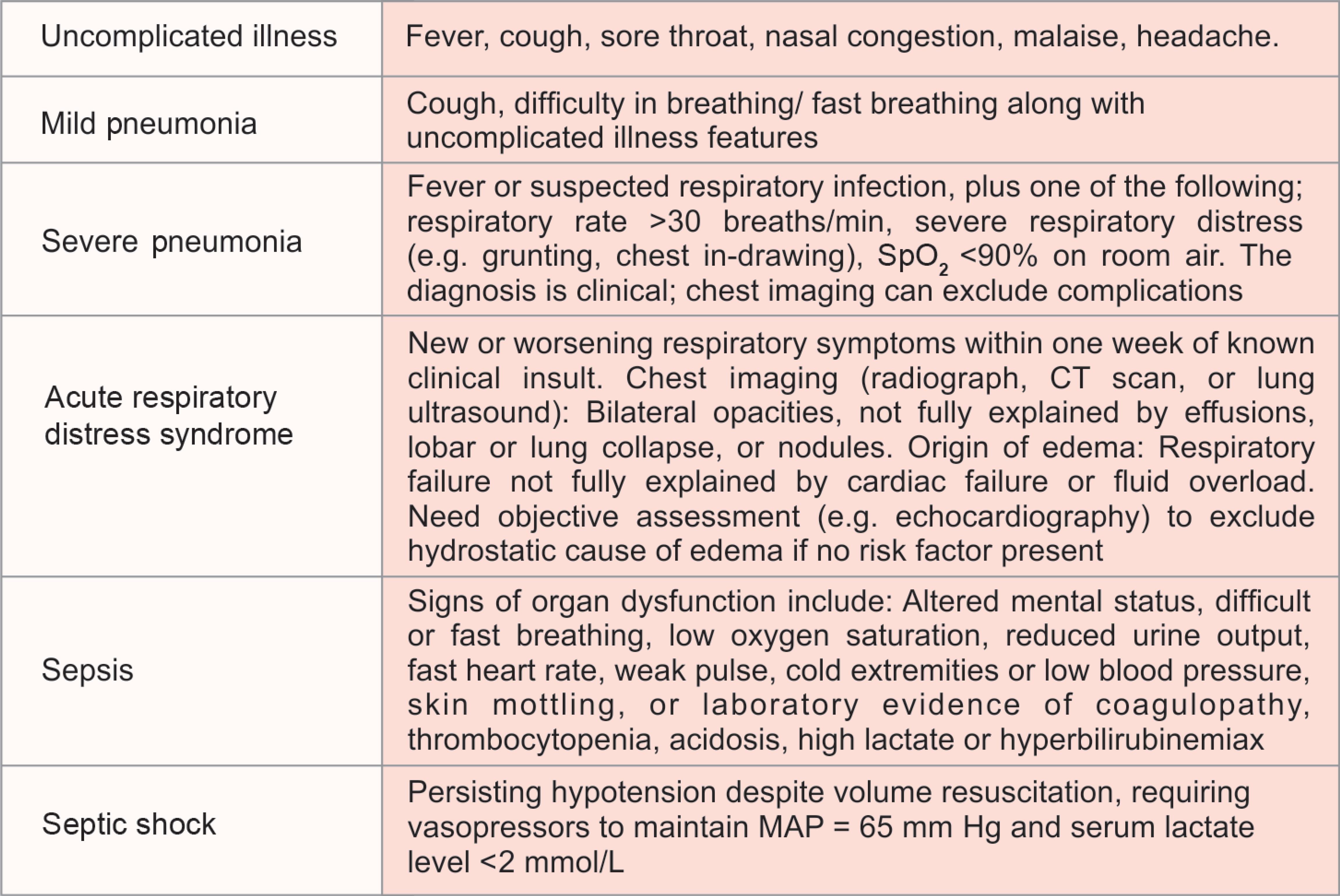
Fig. 1: Clinical syndromes associated with COVID-19
Mild COVID-19 Management: Monitoring and Symptomatic Treatment
- COVID-19 patients with mild symptoms need isolation and can be managed without hospitalization.
- Treat symptomatically with antipyretics for fever. Patients should be counseled about the clinical features of the complicated illness and advised to seek the medical help.
Severe COVID-19 Management: Monitoring and Oxygen Therapy
- Observe the signs of clinical deterioration of progressive respiratory failure, sepsis closely, and treat immediately. Patients with SARI along with no evidence of shock, conservative fluid management should be used cautiously.
- Administer supplemental oxygen therapy (5 L/min) immediately for patients identified with hypoxemia, respiratory distress, SARI, or shock
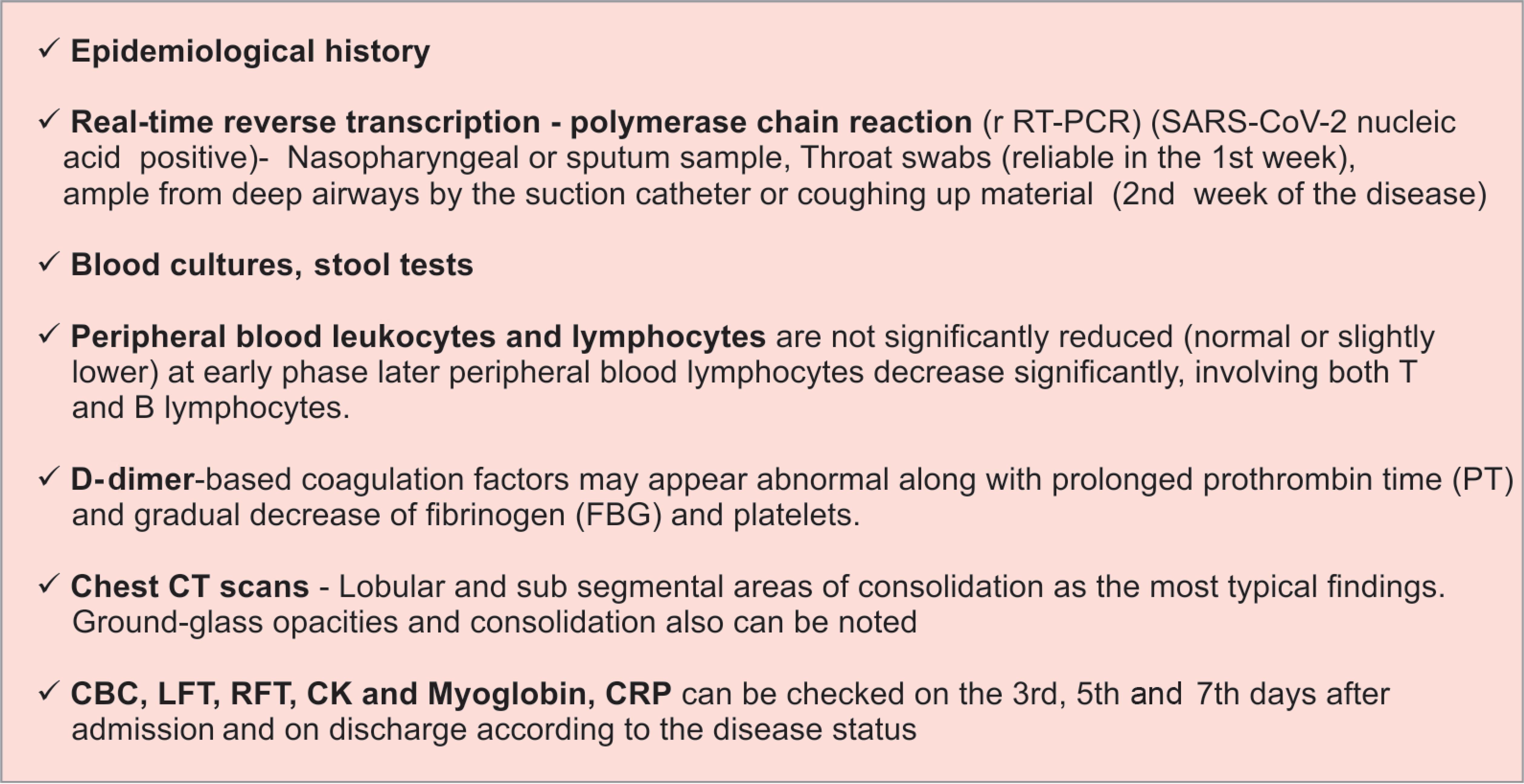
Fig. 2: Diagnostic tests related to COVID-19
Severe COVID-19 Management: Treatment of Coinfections
- Administer antimicrobials/antibiotics to treat pathogens causing SARI and sepsis within one hour of initial assessment of patients with sepsis.
ARDS and Hypoxemic Respiratory Failure Management
- High flow nasal cannula oxygenation (HFNC) or noninvasive mechanical ventilation need to be started. And if the symptoms do not improve, endotracheal intubation and invasive mechanical ventilation need to be initiated.
- Implement mechanical ventilation (prone ventilation for >12 hours per day) using lower tidal volumes (4–8 mL/kg predicted body weight) and lower inspiratory pressures (plateau pressure <30 cm H2O). Deep sedation may be needed. For patients with ARDS (moderate/severe), higher positive end expiratory pressure (PEEP) is recommended instead of lower PEEP.
- Extracorporeal life support (ECLS) or (ECMO) can be performed if needed.
Septic Shock Management
- Standard care includes early recognition of symptoms and start treating within one hour with antimicrobial therapy and fluid loading for hypotension.
- To maintain the mean arterial pressure ≥65 mm Hg and lactate less than 2 mmol/L, in the absence of hypovolemia, vasopressors are recommended. Administer isotonic crystalloid 30 mL/kg in adults in the first three hours as a rapid bolus and up to 40–60 mL/kg in first 1 hour. Do not use hypotonic crystalloids, starches, or gelatins for resuscitation.
Other Therapeutic Measures
- For patients with progressive deterioration of oxygenation indicators, rapid worsening on imaging and excessive activation of the body’s inflammatory response, and glucocorticoids (methylprednisolone 1–2 mg/kg/day) can be used for a short period (3–5 days).
- Oseltamivir 75 mg (BD × 5d), azithromycin 500 mg (OD × 5d), HCQ 400 mg OD on first day, 200 mg BD × 4d are the recommendation in India, unless it is contraindicated for the patients.
Prevention of Complications
| Invasive mechanical ventilation–reduction |
|
| Ventilator-associated pneumonia |
|
| Venous thromboembolism |
|
| Catheter-related bloodstream infection |
|
| Stress ulcers and GI bleeding |
|
| ICU-related weakness |
|
Discharge Criteria from the Hospital15,16
- Patient clinically stable
- Radiologically clear
- Two negative samples taken 24 hours apart
COMPLICATIONS16,19
Respiratory distress syndrome, septic shock, acute liver injury, metabolic acidosis, acute cardiac injury, coagulation dysfunction, and multiorgan failure.
PREVENTIVE MEASURES5,13
- Vaccines are under trial as of now.
- Hygiene (hand, respiratory, and toilet), social distancing, and limiting contact with symptomatic people are the preventive measures to be followed by individuals.
- Appropriate use of PPE and addition of airborne precautions (N95/FFP2/3 if AGP) while performing aerosol-generating procedures need to be followed by the healthcare workers.
REFERENCES
1. https://en.wikipedia.org/wiki/Coronavirus#cite_note-10.
2. Definition of Coronavirus by Merriam-Webster,Merriam-Webster, archived from the original on 2020-03-23, retrieved 2020-03-24.
3. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382(8):727–733. DOI: 10.1056/NEJMoa2001017.
4. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation and Treatment Coronavirus (COVID-19). https://www.ncbi.nlm.nih.gov/books/NBK554776/.
5. Clinical Care for Severe Acute Respiratory InfectionToolkit COVID-19, WHO https://apps.who.int/iris/bitstream/handle/10665/331736/WHO-2019-nCoV-SARI_toolkit-2020.1-eng.pdf?sequence=1andisAllowed=y.
6. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020. DOI: 10.1056/NEJMoa2001316.
7. Coronavirus disease 2019 (COVID-19). Situation Report –66 WHO https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200326-sitrep-66-covid-19.pdf?sfvrsn=81b94e61_2.
8. Guo Y-R, Cao Q-D, Hong Z-S, Tan Y-Y, Chen S-D, Jin H-J, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res 2020;7(1):11. DOI: 10.1186/s40779-020-00240-0.
9. https://www.mayoclinic.org/diseases-conditions/coronavirus/symptoms-causes/syc-20479963.
10. https://www.who.int/health-topics/coronavirus#tab=tab_1.
11. https://www.drugabuse.gov/about-nida/noras-blog/2020/04/covid-19-potential-implications-individuals-substance-use-disorders.
12. Li T, Lu H, Zhang W. Clinical observation and management of COVID-19 patients. Emerg Microbes Infect 2020;9(1):687–690. DOI: 10.1080/22221751.2020.1741327.
13. Rothana HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020;109:102433. DOI: 10.1016/j.jaut.2020.102433.
14. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html.
15. Guidelines on Clinical Management of COVID – 19, Government of India Ministry of Health and Family Welfare Directorate General of Health Services. https://www.mohfw.gov.in/pdf/RevisedNationalClinicalManagementGuidelineforCOVID1931032020.pdf.
16. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance, https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected.
17. Li T, Diagnosis and clinical management of severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection: an operational recommendation of Peking Union Medical College Hospital (V2.0) https://www.tandfonline.com/doi/full/10.1080/22221751.2020.1735265.
18. https://en.wikipedia.org/wiki/COVID-19_testing#cite_note-20200130cdc-9.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.